First 100 Days: Getting America’s Schools & Communities Back on Track through an Early Warning System for COVID-19 and Future Epidemics
PROBLEM
To reopen schools and keep communities healthier, we need an early warning system to better prepare and respond to future outbreaks of COVID-19, pandemic flu, and other new illness strains.
SOLUTION
The U.S. Government can utilize and strengthen existing networks of real-time data, generated from the public’s voluntary use of affordable, trusted sensor technology such as smart thermometers, to improve preparedness for and response to contagious illness, while simultaneously equipping schools with a proven tool to curb transmission and safely reopen.
BENEFIT 1: CURB TRANSMISSION TO HELP SCHOOLS SAFELY REOPEN
With real-time data on how illness starts and spreads, school leaders can make proactive decisions about opening, closing, and other policies, curbing transmision and inspiring confidence that schools are safe.
EXAMPLE: Kinsa’s FLUency program is a proven school health program that reduces the spread of illness in schools and communities through a network of smart thermometers, letting school leaders, parents, and teachers see real-time, grade-by-grade snapshots of illness levels. FLUency has been run in thousands of schools over the past six years, and:
Helps individuals detect and respond to illness early and appropriately.
Guides families on when to keep children at home, reducing classroom transmission.
Empowers parents and administrators with real-time information on what’s going around.
Contains outbreaks through targeted early interventions.
Improves attendance at school while ensuring student, staff and community safety.
BENEFIT 2: IMPROVE COMMUNITY PREPAREDNESS AND RESPONSE
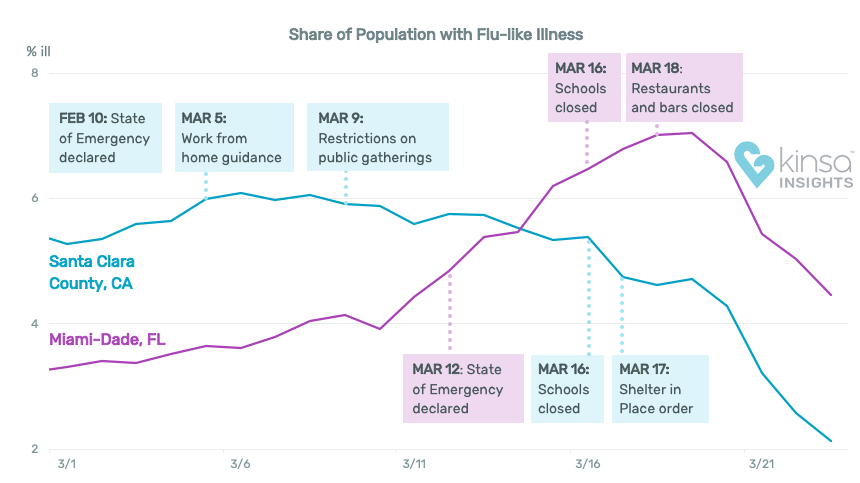
Population-level data aggregated from a nationwide network of smart thermometers (a thermometer connected to an app which provides users with healthcare guidance based on symptom inputs, age, and other relevant information) provides a real-time snapshot of where and when illness is starting and how fast it spreads, painting a granular picture of transmission weeks ahead of other sources. Because products like smart thermometers are used within hours of symptom onset, well before an individual talks to a doctor or seeks care, these products provide far earlier insights than public health systems.
EXAMPLE: With an existing smart thermometer network of two million users, Kinsa detected the emerging pandemic in the U.S. before any other system, and can predict COVID-19 surges up to three weeks and flu up to 20 weeks in advance on a city-by-city basis. This “pre-healthcare” data provides vital insight for federal, state and local leaders to:
Know where symptoms associated with COVID-19 are occurring in real-time
Deploy resources early -- testing, PPE, and other pinpointed public health responses
Contain the outbreak through targeted intervention with the newly ill
Monitor the effectiveness of interventions in real-time
ADVANCING THE BIDEN-HARRIS ADMINISTRATION’S PRIORITIES
Prioritizing an early warning system for outbreaks promotes key tenets of the President-elect’s plan to:
Provide evidence-based guidance for how to turn the dial up or down relative to the level of risk and degree of viral spread in a community, including when to open or close schools and what steps they need to take to make classrooms and facilities safe;
Create a Nationwide Pandemic Dashboard that Americans can check in real-time to help them gauge whether local transmission is actively occurring in their zip codes.
Protect older Americans and others at high risk.
Rebuild and expand defenses to predict, prevent, and mitigate pandemic threats, including those coming from China.
A bipartisan letter supporting the prioritization of an early warning system was recently sent to Congressional leadership, and an early warning system is broadly supported by policy experts and government stakeholders, and is already being deployed in partnership with Connecticut, Colorado, Philadelphia, and other locations. A recent report by Third Way calls for “fund[ing] a national system of early detection using smart thermometers that provide warnings of outbreaks faster than testing” as a top economic recovery priority for 2021. The Bipartisan Policy Center recommends that Congress complement testing with an early warning surveillance system, including “network-connected device systems (e.g., smart thermometers) and wastewater surveillance to locate COVID-19 hot spots and other infectious disease outbreaks.” The FLUency school health program is endorsed by the California School Nurses Organization, the Idaho Education Association, and other education stakeholders. New Orleans Mayor LaToya Cantrell said that the partnership between the City and Kinsa means that “many of our schools…will have the tools to catch the signs of COVID-19 swiftly and accurately."
HOW IT WORKS
PILLAR 1: Help schools reopen safely and reach the communities critical to ending the pandemic.
Eight-five percent of smart thermometers distributed through the FLUency program go to families in Title I, underserved schools. These households often include multigenerational families, first responders, essential workers, and those who lack sufficient access to the health care system. Because the program is grassroots-focused and entirely opt-in, it sees high levels of engagement:
20-25% of households typically opt in to receiving a Kinsa thermometer.
65% of participants are active weekly, sustained throughout the school year.
40% of families did not own a thermometer prior to participating.
The app’s two-way communication channels leverage this strong participation, providing an opportunity to reach key communities with public health messages, information about forthcoming vaccines, and behavioral nudges. Results include:
27% decrease in illness-based school absenteeism during the peak of flu season.1
40% of participants who contract the flu received antivirals within 48 hours.2
21% decrease in unnecessary ER visits (non-injury basis) based on claims data.3
PILLAR 2: Identify unusual illness clusters in advance so experts can investigate.
The arrival of COVID-19 caught the nation by surprise -- in fact, the virus had been spreading in the U.S. undetected for several weeks. By tracking fevers and symptoms as soon as people experience them and comparing population-level data against expected trends, the network alerts public health officials to new outbreaks, allowing them to investigate sooner. Dr. William Schaffner, a professor of preventive medicine at Vanderbilt University, called the use of a network of smart thermometers “21st-century disease surveillance, and we’ve been rooted in the mid-20th century with something very labor intensive.” For example:
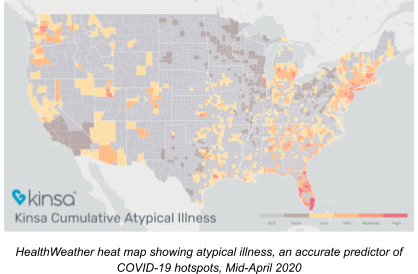
In March, Kinsa used aggregated smart thermometer data to produce a real-time county-level map of unusual fever clusters -- those above and beyond expected cold and flu.
The clusters of unusual fever were verified by top epidemiologists to strongly correlate with COVID-19 outbreaks occurring approximately three weeks later.
This data proved to be an accurate early warning signal of COVID-19 case surges.
PILLAR 3: Predict how known epidemics will spread and determine if containment measures are working.
This network of smart thermometers can predict, down to the city level, the incidence of flu up to 20 weeks in advance. This is in contrast to the next best, a CDC Influenza Forecasting Center of Excellence (Carnegie Mellon University), which can model flu spread three weeks in advance and at the state or multi-state level. Dr. Benjamin Dalziel of Oregon State University, a rising researcher in infectious disease forecasting, called Kinsa’s data “by far the most high-quality data set I’ve ever worked with.”
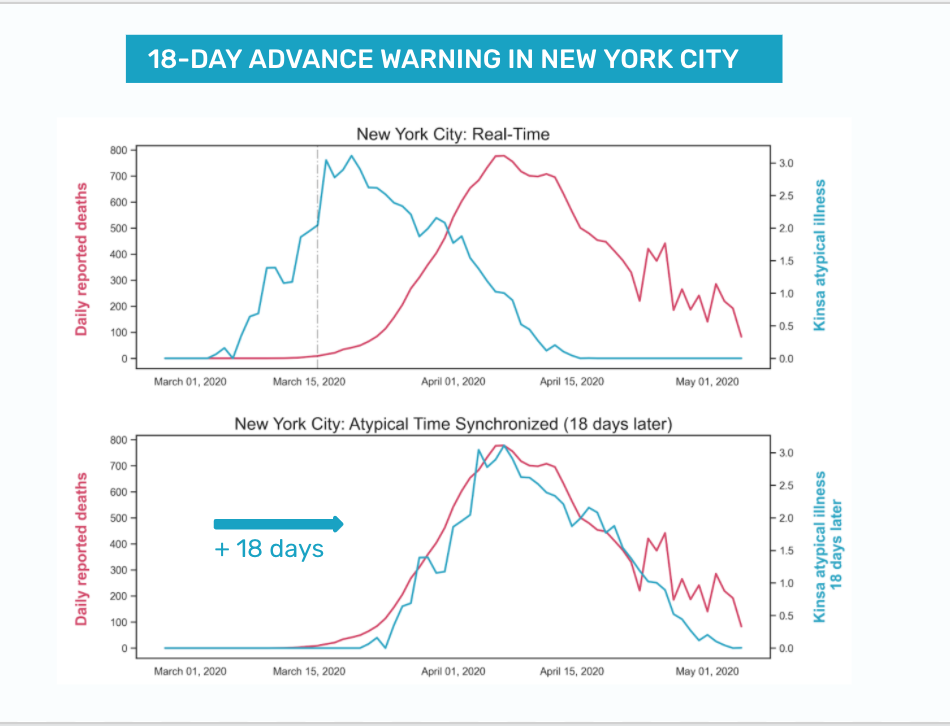
With earlier warning, public health officials can more effectively target resources while minimizing burdens on unaffected areas. In addition, they can see the impact of interventions in real time. By way of example:
In New York City, Kinsa’s data showed the shutdown was turning the tide five days before the City’s own data -- a critical window to assess the efficacy of those restrictions.
This spring, as 248 million Americans in at least 29 states were told to stay at home, Kinsa has been providing data to officials in five states and three cities to identify future spikes and determine whether (and how quickly) mitigation measures were breaking the chain of infection.
Columbia University researchers found that if New York City had responded even one week earlier, it would have prevented more than 200,000 cases. Based on the rate and cost of hospitalization due to COVID-19, those cases cost nearly $1B USD. By contrast, the cost of Kinsa's existing sensor network in New York City -- which detected the outbreak far earlier than other sources -- was just $300K USD. Deploying Kinsa’s recommended level of thermometers to enable even earlier and more geographically precise surveillance would cost less than $6M USD. When compared with the above cost of preventable cases, this investment would generate an ROI of nearly 200x for the first wave of COVID-19 cases alone.
RECOMMENDATIONS
Direct HHS and CDC to prioritize early warning systems for outbreaks and modernize public health surveillance tools to include network-connected devices.
Utilize and strengthen existing early detection networks.
Knowing where and when outbreaks are occurring in real time is critical for a robust response. Partnerships with the private sector can bring this information and insight, gleaned from years of proprietary, historical illness data and analysis, to the federal government quickly and affordably. Kinsa’s ability to detect atypical illness and accurately predict flu incidence up to 20 weeks in advance offers a major advantage compared with the Government’s current capabilities, but a modest investment (less than $150 million) to distribute additional smart thermometers (primarily through schools) to enhance the network would allow for zip code-level forecasting in population centers while reaching the populations key to epidemic control.Focus network growth in key populations: the underserved, schools, & seniors.
Funding the deployment of products like smart thermometers via U.S. public schools is an immediate way to expand the network in key populations and grow an early warning system. For example, Kinsa’s FLUency school health program, which targets Title I school communities and is run in 5% of U.S. elementary schools today, has been shown to improve health outcomes, decrease illness-based absenteeism, increase healthy behaviors, and enable schools to re-open safely. This program reaches underserved communities, essential workers, multi-generational families, and others at high risk to contract and spread illness. Additionally, seniors are especially vulnerable to epidemics, and there has been a surge in this use of products like smart thermometers by this demographic since the beginning of the pandemic -- demonstrating the potential for broad adoption. Although nearly 17,000 U.S. elementary schools (~20% of the U.S.) have applied for this program, Kinsa has funding for only 4,000 schools. Funding FLUency in America’s schools will help schools safely reopen while supporting key tenets of the President-elect’s plan to respond according to the degree of risk and viral spread.Clarify BARDA’s authority to fund population-level early warning technology.
Previously, Kinsa was informed by BARDA representatives in July 2020 that current regulations allow funding only for individual-level diagnostic tools, not population level early warning. However, the ability to support population-level early warning systems would help state and local officials better predict, prepare, and evaluate outbreak response effectiveness.
This is an unprecedented opportunity to protect public health, bolster the economy, and create a world-class outbreak early warning system that demonstrates a commitment to our most vulnerable citizens and to saving lives and livelihoods, while driving a substantial return on investment.
FAQ & APPENDIX
Q: Not everyone experiences fever as a COVID symptom. Why is a thermometer useful for capturing transmission of illness? Won’t it miss a lot of cases?
We don’t need every COVID-19 patient to have a fever to see how illness is spreading across a population in real time. Similar to testing, even if not everyone gets a test, the number of people who do test lets us estimate how much illness is in the population. For example, if 50% of COVID-19 patients experience a fever, a doubling of people with fever in a particular location means that the same proportion were likely infected in that time period but did not get a fever. Between March 1 and November 1, Kinsa captured nearly 15 million fever readings and 1.7 million symptom inputs.
Q: What are the privacy implications of sharing this data?It is possible to both protect personal privacy and also gather and share the information necessary to detect and effectively respond to outbreaks like COVID-19. For example, Kinsa shares population health insights -- i.e., the percentage of people in a county who are ill. There is no way to identify an individual from this illness signal.
Q: Why does Kinsa focus on schools?
Schools are a gateway to reach larger household sizes and traditionally underserved communities. Additionally, schools play a central role within communities, and promoting outbreak detection in schools effectively helps detect outbreaks in the broader community. For the past five years, Kinsa’s school health program has sustained high levels of engagement amongst participants, with 65% of participants viewing and contributing to health trends weekly. We’ve seen that the program reduces illness in schools by guiding families to earlier care and treatment, directing symptomatic students and staff to stay home, and increasing preventive behaviors of those at-risk. Past results of this program include a 27% decrease in illness-based school absenteeism during the peak of flu season.
EXPERT SUPPORT OF THE KINSA EARLY WARNING SYSTEM
William Schaffner, MD, Professor of Preventive Medicine, Vanderbilt University
Peter J. Hotez, MD PhD, Dean, Nat’l School of Tropical Medicine, Baylor College of Medicine
Nirav Shah, MD MPH, Sr Scholar, Stanford University, Former NY State Health Commissioner
"Real-time fever data 'could speed up public health the way Twitter sped up the news cycle.’” (NYT, March 18, 2020)
“CDC predicts the flu for three weeks out. This company has cracked the code on predicting flu 20 or more weeks away in the future.” (Inside Health Policy, April 6, 2020)
Data from private companies like Unacast and Kinsa could work for short-term decision-making in the health care community, but also eventually be built into a bigger national surveillance system. (Inside Health Policy, April 6, 2020)
Benjamin Dalziel, PhD, Oregon State University
"The company’s thermometer readings 'are by far the most high-quality data set I’ve ever worked with.’” (NYT, March 18, 2020)
KINSA EARLY WARNING SIGNAL: SCIENCE AND PROOF POINTS
See here for a summary of the latest science, analysis and publications.
- Research study conducted in 3 test schools and 3 control schools in Utah.
- Survey results, Kinsa users.
- Two-armed study conducted with a top 5 national health insurer.

